Abstract
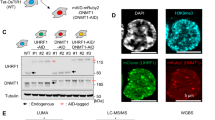
Although the majority of patients with acute myeloid leukemia (AML) initially respond to chemotherapy, many of them subsequently relapse, and the mechanistic basis for AML persistence following chemotherapy has not been determined. Recurrent somatic mutations in DNA methyltransferase 3A (DNMT3A), most frequently at arginine 882 (DNMT3AR882), have been observed in AML1,2,3 and in individuals with clonal hematopoiesis in the absence of leukemic transformation4,5. Patients with DNMT3AR882 AML have an inferior outcome when treated with standard-dose daunorubicin-based induction chemotherapy6,7, suggesting that DNMT3AR882 cells persist and drive relapse8. We found that Dnmt3a mutations induced hematopoietic stem cell expansion, cooperated with mutations in the FMS-like tyrosine kinase 3 gene (Flt3ITD) and the nucleophosmin gene (Npm1c) to induce AML in vivo, and promoted resistance to anthracycline chemotherapy. In patients with AML, the presence of DNMT3AR882 mutations predicts minimal residual disease, underscoring their role in AML chemoresistance. DNMT3AR882 cells showed impaired nucleosome eviction and chromatin remodeling in response to anthracycline treatment, which resulted from attenuated recruitment of histone chaperone SPT-16 following anthracycline exposure. This defect led to an inability to sense and repair DNA torsional stress, which resulted in increased mutagenesis. Our findings identify a crucial role for DNMT3AR882 mutations in driving AML chemoresistance and highlight the importance of chromatin remodeling in response to cytotoxic chemotherapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Cancer Genome Atlas Research Network. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074 (2013).
Ley, T.J. et al. DNMT3A mutations in acute myeloid leukemia. N. Engl. J. Med. 363, 2424–2433 (2010).
Yan, X.J. et al. Exome sequencing identifies somatic mutations of DNA methyltransferase gene DNMT3A in acute monocytic leukemia. Nat. Genet. 43, 309–315 (2011).
Genovese, G. et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N. Engl. J. Med. 371, 2477–2487 (2014).
Jaiswal, S. et al. Age-related clonal hematopoiesis associated with adverse outcomes. N. Engl. J. Med. 371, 2488–2498 (2014).
Patel, J.P. et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N. Engl. J. Med. 366, 1079–1089 (2012).
Sehgal, A.R. et al. DNMT3A mutational status affects the results of dose-escalated induction therapy in acute myelogenous leukemia. Clin. Cancer Res. 21, 1614–1620 (2015).
Shlush, L.I. et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature 506, 328–333 (2014).
Leiserson, M.D. et al. Pan-cancer network analysis identifies combinations of rare somatic mutations across pathways and protein complexes. Nat. Genet. 47, 106–114 (2015).
Welch, J.S. et al. The origin and evolution of mutations in acute myeloid leukemia. Cell 150, 264–278 (2012).
Busque, L. et al. Recurrent somatic TET2 mutations in normal elderly individuals with clonal hematopoiesis. Nat. Genet. 44, 1179–1181 (2012).
Jan, M. et al. Clonal evolution of preleukemic hematopoietic stem cells precedes human acute myeloid leukemia. Sci. Transl. Med. 4, 149ra118 (2012).
Challen, G.A. et al. Dnmt3a is essential for hematopoietic stem cell differentiation. Nat. Genet. 44, 23–31 (2011).
Moran-Crusio, K. et al. Tet2 loss leads to increased hematopoietic stem cell self-renewal and myeloid transformation. Cancer Cell 20, 11–24 (2011).
Quivoron, C. et al. TET2 inactivation results in pleiotropic hematopoietic abnormalities in mouse and is a recurrent event during human lymphomagenesis. Cancer Cell 20, 25–38 (2011).
Li, Z. et al. Deletion of Tet2 in mice leads to dysregulated hematopoietic stem cells and subsequent development of myeloid malignancies. Blood 118, 4509–4518 (2011).
Yang, L., Rau, R. & Goodell, M.A. DNMT3A in haematological malignancies. Nat. Rev. Cancer 15, 152–165 (2015).
Holz-Schietinger, C., Matje, D.M. & Reich, N.O. Mutations in DNA methyltransferase (DNMT3A) observed in acute myeloid leukemia patients disrupt processive methylation. J. Biol. Chem. 287, 30941–30951 (2012).
Russler-Germain, D.A. et al. The R882H DNMT3A mutation associated with AML dominantly inhibits wild-type DNMT3A by blocking its ability to form active tetramers. Cancer Cell 25, 442–454 (2014).
Kim, S.J. et al. A DNMT3A mutation common in AML exhibits dominant-negative effects in murine ES cells. Blood 122, 4086–4089 (2013).
Papaemmanuil, E. et al. Genomic classification and prognosis in acute myeloid leukemia. N. Engl. J. Med. 374, 2209–2221 (2016).
Gaidzik, V.I. et al. Clinical impact of DNMT3A mutations in younger adult patients with acute myeloid leukemia: results of the AML Study Group (AMLSG). Blood 121, 4769–4777 (2013).
Ostronoff, F. et al. Mutations in the DNMT3A exon 23 independently predict poor outcome in older patients with acute myeloid leukemia: a SWOG report. Leukemia 27, 238–241 (2013).
Ribeiro, A.F. et al. Mutant DNMT3A: a marker of poor prognosis in acute myeloid leukemia. Blood 119, 5824–5831 (2012).
Tie, R. et al. Association between DNMT3A mutations and prognosis of adults with de novo acute myeloid leukemia: a systematic review and meta-analysis. PLoS One 9, e93353 (2014).
Chen, X. et al. Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. J. Clin. Oncol. 33, 1258–1264 (2015).
Ganzel, C. et al. Minimal residual disease assessment by flow cytometry in AML is an independent prognostic factor even after adjusting for cytogenetic/molecular abnormalities. Blood 124, 1016 (2014).
Ivey, A. et al. Assessment of minimal residual disease in standard-risk AML. N. Engl. J. Med. 374, 422–433 (2016).
Othus, M. et al. Effect of measurable ('minimal') residual disease (MRD) information on prediction of relapse and survival in adult acute myeloid leukemia. Leukemia 30, 2080–2083 (2016).
Walter, R.B. et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative allogeneic hematopoietic cell transplantation. Leukemia 29, 137–144 (2015).
Shih, A.H. et al. Mutational cooperativity linked to combinatorial epigenetic gain of function in acute myeloid leukemia. Cancer Cell 27, 502–515 (2015).
Akalin, A. et al. Base-pair resolution DNA methylation sequencing reveals profoundly divergent epigenetic landscapes in acute myeloid leukemia. PLoS Genet. 8, e1002781 (2012).
Garrett-Bakelman, F.E. et al. Enhanced reduced representation bisulfite sequencing for assessment of DNA methylation at base pair resolution. J. Vis. Exp. http://dx.doi.org/10.3791/52246, e52246 (2015).
Yang, F., Teves, S.S., Kemp, C.J. & Henikoff, S. Doxorubicin, DNA torsion, and chromatin dynamics. Biochim. Biophys. Acta 1845, 84–89 (2014).
Stracker, T.H., Usui, T. & Petrini, J.H. Taking the time to make important decisions: the checkpoint effector kinases Chk1 and Chk2 and the DNA damage response. DNA Repair (Amst.) 8, 1047–1054 (2009).
Collins, A.R. et al. The comet assay: topical issues. Mutagenesis 23, 143–151 (2008).
Pang, B. et al. Drug-induced histone eviction from open chromatin contributes to the chemotherapeutic effects of doxorubicin. Nat. Commun. 4, 1908 (2013).
Dinant, C. et al. Enhanced chromatin dynamics by FACT promotes transcriptional restart after UV-induced DNA damage. Mol. Cell 51, 469–479 (2013).
Ransom, M., Dennehey, B.K. & Tyler, J.K. Chaperoning histones during DNA replication and repair. Cell 140, 183–195 (2010).
Belotserkovskaya, R. et al. FACT facilitates transcription-dependent nucleosome alteration. Science 301, 1090–1093 (2003).
Mayle, A., Luo, M., Jeong, M. & Goodell, M.A. Flow cytometry analysis of murine hematopoietic stem cells. Cytometry A 83, 27–37 (2013).
Akashi, K., Traver, D., Miyamoto, T. & Weissman, I.L. A clonogenic common myeloid progenitor that gives rise to all myeloid lineages. Nature 404, 193–197 (2000).
Chen, K. et al. Resolving the distinct stages in erythroid differentiation based on dynamic changes in membrane protein expression during erythropoiesis. Proc. Natl. Acad. Sci. USA 106, 17413–17418 (2009).
Socolovsky, M. et al. Ineffective erythropoiesis in Stat5a−/−5b−/− mice due to decreased survival of early erythroblasts. Blood 98, 3261–3273 (2001).
Paietta, E. Should minimal residual disease guide therapy in AML? Best Pract. Res. Clin. Haematol. 28, 98–105 006 (2015).
Paietta, E. Minimal residual disease in acute myeloid leukemia: coming of age. Hematology (Am Soc Hematol Educ Program) 2012, 35–42 (2012).
Cheng, D.T. et al. Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets (MSK-IMPACT): A hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17, 251–264 (2015).
Nguyen, S., Meletis, K., Fu, D., Jhaveri, S. & Jaenisch, R. Ablation of de novo DNA methyltransferase Dnmt3a in the nervous system leads to neuromuscular defects and shortened lifespan. Dev. Dyn. 236, 1663–1676 (2007).
Havre, P.A., Yuan, J., Hedrick, L., Cho, K.R. & Glazer, P.M. p53 inactivation by HPV16 E6 results in increased mutagenesis in human cells. Cancer Res. 55, 4420–4424 (1995).
Whitfield, M.L. et al. Identification of genes periodically expressed in the human cell cycle and their expression in tumors. Mol. Biol. Cell 13, 1977–2000 (2002).
Wysocka, J. Identifying novel proteins recognizing histone modifications using peptide pull-down assay. Methods 40, 339–343 (2006).
Westfall, P.H. & Young, S.S. P-value adjustments for multiple tests in multivariate binomial models. J. Am. Stat. Assoc. 84, 780–786 (1989).
Acknowledgements
The authors are grateful to A. Ringler, C. Sheridan, J. Gandara and Y. Neelamraju for technical support; to Weill Cornell Medicine Epigenomics Core for sequencing services; to H. Erdjument-Bromage for assistance with proteomics; to S. Zha (Columbia University Medical Center); and to A. Ciccia (Columbia University Medical Center) for critical reading of the manuscript and helpful suggestions. cDNA encoding human wild-type DNMT3A was a kind gift from F. Fuks (Free University of Brussels). This work was supported by NCI K99 grant CA178191 and Lauri Strauss Leukemia Foundation award to O.A.G.; by NCI K08 grant CA169055 and an American Society of Hematology (ASHAMFDP-20121) under the ASH-AMFDP partnership with The Robert Wood Johnson Foundation to F.E.G.-B.; by a Hyundai Hope On Wheels award to B.S.; by a Gabrielle's Angel Fund grant to R.L.L. and A.M.M.; by NCI grant CA172636 to R.L.L. and A.M.M.; by the Samuel Waxman Cancer Research Center; by a Stand Up To Cancer Convergence Award to R.L.L; and the NCI U10 grant CA180827 to E.M.P., R.L.L. and A.M.M. A.S.M. is supported by NIH grants T32GM007739 and F30CA18349. A.M.M. is a Burroughs Wellcome Clinical Translational Scholar, and is supported by the Sackler Center for Biomedical and Physical Sciences. R.L.L. is a LLS Scholar. P.B.S. is supported by the Austrian Research Foundation (#P27132) and the Oesterreichische Nationalbank (OeNB) Anniversary Fund (#15936). MSKCC cores used in these studies are supported by the P30 Core Grant CA008748. A part of this study was coordinated by the ECOG-ACRIN Cancer Research Group (R.L. Comis and M.D. Schnall) and supported in part by Public Health Service Grants CA180820, CA180794, CA180791, CA189859, CA180827 and from the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Its content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute.
Author information
Authors and Affiliations
Contributions
O.A.G. and K.S. performed most of the experiments. L.B., M.D.K., D.T., E.L., A.R.W., A.R.G., E.P., F.P. and A.S.M. assisted with many of the experiments. C.Z., J.M.R., M.S.T., O.A.-W., M.G., E.M.P., A.M.M. and R.L.L. designed the clinical study, and collected and analyzed patient data. A.G.C., A.V.K., R.P.K. and S.A.A. designed, conducted and analyzed ChIP-sequencing experiments. B.S., F.E.G.-B. and A.M.M. assisted with RNA-sequencing, ERRBS and data analysis. B.S. mined TCGA data. L.L. and S.D.N. designed and performed peptide pull-down assay. B.H.D. assisted with animal hematopathology. A.M. and M.E.A. assisted with patient DNA re-sequencing. G.H., W.R.S., S.K. and P.B.S. designed and conducted ex vivo drug studies on primary AML samples. J.R.C. designed and oversaw small-molecule quantification by mass-spectroscopy. S.A.R., Y.K.L. and S.M. provided Dnmt3a cKO mice, S.M. contributed to study conception. O.A.-W. assisted with study design. O.A.G. and R.L.L. conceived the study, designed experiments, analyzed data and wrote the manuscript. All of the authors read, edited and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–8 and Supplementary Tables 1–3, 7, 8 (PDF 15780 kb)
Supplementary Table 4
Differentially methylated cytosines (DMCs) in LSK cells from Dnmt3amut mice compared to wild-type controls, identified by MethyKit (XLSX 1235 kb)
Supplementary Table 5
Differentially expressed genes in LSK cells from Dnmt3amut mice compared to wild-type controls, identified by RNA-seq. (XLSX 58 kb)
Supplementary Table 6
Candidate DNMT3A interacting proteins identified by mass-spectroscopy following DNMT3A peptide pull-down. (XLSX 56 kb)
Rights and permissions
About this article
Cite this article
Guryanova, O., Shank, K., Spitzer, B. et al. DNMT3A mutations promote anthracycline resistance in acute myeloid leukemia via impaired nucleosome remodeling. Nat Med 22, 1488–1495 (2016). https://doi.org/10.1038/nm.4210
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4210
This article is cited by
-
Clonal medicine targeting DNA damage response eradicates leukemia
Leukemia (2024)
-
Epigenetic regulation in hematopoiesis and its implications in the targeted therapy of hematologic malignancies
Signal Transduction and Targeted Therapy (2023)
-
Cre recombinase expression cooperates with homozygous FLT3 internal tandem duplication knockin mouse model to induce acute myeloid leukemia
Leukemia (2023)
-
Measurable residual disease detected by flow cytometry independently predicts prognoses of NPM1-mutated acute myeloid leukemia
Annals of Hematology (2023)
-
DNMT3A R882H mutation drives daunorubicin resistance in acute myeloid leukemia via regulating NRF2/NQO1 pathway
Cell Communication and Signaling (2022)