Abstract
Hypertension is a principal cause of mortality and morbidity in Singapore. The use of home blood-pressure monitoring (HBPM) to assess hypertensive control with digital devices in the local multi-racial population is unknown. The study determined the factors associated with hypertensive patients’ use of HBPM in primary care in a multi-racial Asian population. Randomized cross-sectional questionnaire survey of hypertensive patients managed in a district polyclinic. A model predicting use of HBPM was constructed by univariate and multivariate logistic regression. A total of 224 eligible subjects were randomly selected from 1943 patients. Response rate was 78.1% (n=175). In all, 61.7% of them were aware of HBPM but only 24% used HBPM. Using multivariate analysis by stepwise backward regression, the final fitted model showed that HBPM was associated with higher patients’ socioeconomic status: (adjusted OR for middle-income status=2.85, 95% CI: 1.2–6.78, P=0.018; adjusted OR for high-income status=3.46, 95% CI: 1.22–9.87, P=0.020) and their documented diastolic BP (adjusted OR for diastolic BP>80 mmHg=2.26, 95% CI: 1.06–4.82, P=0.034). Nonusers cited failure to recognize benefits (54.1%), lack of HBPM awareness (29.3%), understanding of device operation (18.8%) and perception of inaccuracy (10.5%) as deterrents. 76.2% of users were satisfied with HBPM but lacked knowledge in maintenance of devices. In conclusion, 61.7% of the study population were aware of HBPM but only 24% used it. Patients’ failure to recognize benefits, lack of awareness, cost and perception of inaccuracy were barriers. Higher socioeconomic status and patient's documented diastolic BP correlated with HBPM usage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ministry of Health Singapore. Health Facts Singapore 2004. Statistics, Publications & Resources: Ministry of Health Singapore, 2004. http://www.moh.gov.sg/corp/publications/list.do?id=pub_reports.
Geok LB . Census of Population 2000. Geographical Distribution and Travel Statistical Release 4. Singapore Department of Statistics, Ministry of Trade and Industry: Singapore, 2000.
Hahn LP et al. Prevalence and accuracy of home sphygmomanometers in an urban population. Am J Public Health 1987; 77: 1459–1461.
Krecke HJ, Fleischmann C, Bokmann M . Distribution and acceptance of self-measurement of blood pressure in the Hamburg area. Schweiz Rundsch Med Prax 1989; 78: 1336–1342.
Jeck T et al. Performing self-measurement of blood pressure: a patient survey. Schweiz Rundsch Med Prax 1991; 80: 456–461.
Tsuji I et al. Proposal of reference values for home blood pressure measurement: prognostic criteria based on a prospective observation of the general population in Ohasama, Japan. Am J Hypertens 1997; 10 (4 part 1): 409–418.
Kleinkert HD et al. What is the value of home blood pressure measurement in patients with mild hypertension? Hypertension 1984; 6: 574–578.
Yarows SA, Julius S, Pickering TG . Home Blood Pressure Monitoring. Arch Intern Med 2000; 160: 1251–1257.
Bailey RH, Knaus VL, Bauer JH . Aneroid sphygmomanometers: an assessment of accuracy at a university hospital and clinics. Arch Intern Med 1991; 151: 1409–1412.
Stergiou GS et al. Home self-monitoring of blood pressure: is fully automated oscillometric technique as good as conventional stethoscopic technique? Am J Hypertens 1997; 10 (4 part 1): 428–433.
Sega G et al. Ambulatory and home blood pressure normality: the PAMELA study. J Cardiovasc Pharmacol. 1994; 23 (Suppl 5): S12–S15.
Staessen J et al. Reference values for the ambulatory blood pressure and the blood pressure measured at home: a population study. J Hum Hypertens 1991; 5: 355–361.
Bialy GB et al. Comparison of office, home and 24-hour ambulatory blood pressures in borderline and mild hypertension. Angiology 1988; 39: 752–760.
Association for the Advancement of Medical Instrumentation. Electronic or Automated Sphygmomanometers. Arlington, VA: American National Standards Institute Inc, 1992, pp 1–40.
O’Brien E et al. Short report: an outline of the revised British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens 1993; 11: 677–679.
Weber F et al. Comparative clinical study on the accuracy of conventional and electronic blood pressure self-measuring devices. Z Kardiol 1981; 70: 700–705.
Harrison DW, Kelly PL . Home health-care: accuracy, calibration, exhaust and failure rate comparisons of digital blood pressure monitors. Med Instrum 1987; 21: 323–328.
Soghikan K et al. Home blood pressure monitoring: effect on use of medical services and medical costs. Med Care 1992; 30: 855–865.
Stahl SM et al. Effects of home blood pressure measurement on long term control. Am J Public Health 1984; 74: 704–709.
Zarnke KB, Feagan BG, Mahon JL, Feldman RD . A randomized study comparing a patient-directed hypertension strategy with usual office-based care. Am J Hypertens 1997; 10: 58–67.
Acknowledgements
We were grateful to the nurses, Vasanti, Violet and Mary, who rendered their assistance in data entry and the team of research nurses who interviewed the subjects in their residence. The study was supported by a small research grant from CTERU/NMRC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tan, N., Khin, L. & Pagi, R. Home blood-pressure monitoring among hypertensive patients in an Asian population. J Hum Hypertens 19, 559–564 (2005). https://doi.org/10.1038/sj.jhh.1001865
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001865
Keywords
This article is cited by
-
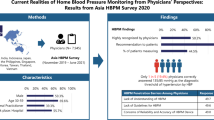
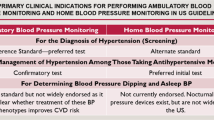
Current realities of home blood pressure monitoring from physicians’ perspectives: results from Asia HBPM survey 2020
Hypertension Research (2023)
-
Factors influencing home blood pressure monitor ownership in a large clinical trial
Journal of Human Hypertension (2022)
-
The influence of self-owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: A qualitative study
BMC Family Practice (2011)
-
Home blood pressure measurements associated with better blood pressure control: the J-HOME study
Journal of Human Hypertension (2008)
-
Home blood pressure measurement: a means for improving blood pressure control?
Journal of Human Hypertension (2008)