Abstract
OBJECTIVE
Use of cardiac devices has been increasing rapidly along with concerns over their safety and effectiveness. This study used hospital administrative data to assess cardiac device implantations in the United States, selected perioperative outcomes, and associated patient and hospital characteristics.
METHODS
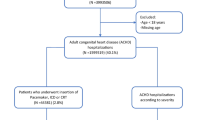
We screened hospital discharge abstracts from the 1997–2004 Healthcare Cost and Utilization Project Nationwide Inpatient Samples. Patients who underwent implantation of pacemaker (PM), automatic cardioverter/defibrillator (AICD), or cardiac resynchronization therapy pacemaker (CRT-P) or defibrillator (CRT-D) were identified using ICD-9-CM procedure codes. Outcomes ascertainable from these data and associated hospital and patient characteristics were analyzed.
MEASUREMENTS AND MAIN RESULTS
Approximately 67,000 AICDs and 178,000 PMs were implanted in 2004 in the United States, increasing 60% and 19%, respectively, since 1997. After FDA approval in 2001, CRT-D and CRT-P reached 33,000 and 7,000 units per year in the United States in 2004. About 70% of the patients were aged 65 years or older, and more than 75% of the patients had 1 or more comorbid diseases. There were substantial decreases in length of stay, but marked increases in charges, for example, the length of stay of AICD implantations halved (from 9.9 days in 1997 to 5.2 days in 2004), whereas charges nearly doubled (from $66,000 in 1997 to $117,000 in 2004). Rates of in-hospital mortality and complications fluctuated slightly during the period. Overall, adverse outcomes were associated with advanced age, comorbid conditions, and emergency admissions, and there was no consistent volume–outcome relationship across different outcome measures and patient groups.
CONCLUSIONS
The numbers of cardiac device implantations in the United States steadily increased from 1997 to 2004, with substantial reductions in length of stay and increases in charges. Rates of in-hospital mortality and complications changed slightly over the years and were associated primarily with patient frailty.
Similar content being viewed by others
Pacemakers (PMs), automatic implantable cardioverter-defibrillators (AICDs), and cardiac resynchronization therapy systems (CRTs) are medical devices that regulate cardiac rate and rhythm and coordinate myocardial contraction.1 Overall, these cardiac devices have been shown to improve symptoms, quality of life, and survival,2,3 fueling increasing enthusiasm for their use.4–8 The increased use, along with concerns about safety and effectiveness of the devices and the financial incentives associated with their use, has increased the need for data to track utilization and outcomes.
Multiple sources of data on cardiac devices exist. First, clinical trials are continually being conducted to study new indications and technologies.3,9–13 Second, reports of case series and retrospective reviews of medical records at local institutions offer lessons learned from practice about operative procedures and prevention of complications.14–18 Third, device registries have been established to collect information on devices, operators, and implantation techniques, as well as on some aspects of outcomes.19 For example, the Center for Medicare & Medicaid Services (CMS) established an AICD registry in January 2005 and required hospitals to submit data on every implantation for Medicare payment.20,21 Fourth, the Food and Drug Administration (FDA), through MedSun and other reporting mechanisms, collects data from operators and manufacturers on device flaws, malfunctions, and adverse events, and issues advisories and recalls.22–26 Fifth, surveys of operators and manufacturers have been conducted to monitor use in the Unites States4,5,27 and worldwide.28 Lastly, administrative data or hospital claims data have been used to track utilization in broad patient populations.6,7
Each of these data sources has advantages and weakness. Clinical trials provide robust data on efficacy, but are limited by their choice of patients and clinical settings. Case reports and retrospective reviews are rooted in real experience, but are limited in generalizability and by the size of observation sets. Registries usually have narrow focuses, such as on device flaws and malfunction. FDA voluntary reports are limited to what is voluntarily reported. Although lacking in clinical details and susceptible to coding errors, administrative data have several advantages over other data sources: primarily large size and nationwide coverage.29 Administrative data-based analysis is a convenient and efficient method when properly approached and can provide valuable information to supplement surveys, registries, case series, and clinical trials to study utilization, patient and hospital characteristics, patient outcomes, and associated factors.
This study explores the use of nationwide administrative data to assess the incidence of PM, AICD and CRT implantations, patient and hospital characteristics, selected perioperative outcomes, and relationships between them for the period 1997–2004. This study does not address clinical indications or the clinical benefits of the devices because of the nature of the data but rather focuses on nationwide utilization, characteristics and outcomes ascertainable from administrative data to provide a comprehensive scan of cardiac device utilization in the United States and pave the way for refined analyses that focus on specific clinical issues.
METHODS
Data and Variables
The primary source of data for this study was the 1997–2004 Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Samples (NIS) developed by the Agency for Healthcare Research and Quality (AHRQ).30 Each annual sample contained about 8 million uniform hospital discharge abstracts from more than 900 short-term general hospitals across more than 30 participating states, approximating a 20% stratified sample of nonfederal acute care hospitals in the United States. NIS includes variables on source and type of admission, 15 diagnosis codes as classified in the International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM), 15 ICD-9-CM procedure codes, procedure days from admission, discharge status, length of stay (LOS), total charges, patient demographic characteristics, insurance coverage, and a few hospital characteristic variables (e.g., hospital procedure volume, size, ownership, and location). The database also included sampling weights and design variables for generating national estimates.
Three additional variables—costs, comorbidities, and hospital volume—were created based on variables from HCUP data. Hospital-specific cost-to-charge ratios, developed by HCUP,30 were used to convert charges to costs. The Elixhauser method31 was used to define 30 comorbid diseases based on diagnosis codes. Defining hospital volume was not as straightforward. Despite recognition of the importance of surgeon procedure volume,32–34 no agreement exists as to what constitutes high, medium, or low volume. Furthermore, because NIS does not identify surgeons, only hospital volume could be constructed. Based on the literature and initial exploration of the data, we summed the number of elective total cardiac device implantations performed, including primary systems of pacemaker, CRT, and AICD, by each hospital to categorize hospital volume. A “low-volume hospital” performed fewer than 100 new cardiac device implantations; a “high-volume hospital” performed 300 or more.
Identification of Patients with Cardiac Device Implantation
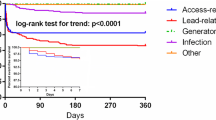
Cardiac device implantation was identified from ICD-9-CM procedure codes. Initial exploration showed that of 71,201 discharges with cardiac device procedure codes in the 2003 NIS, 37% had 1 code, 60% had 2, and 3% had 3 to 5 cardiac device procedure codes. The Appendix classifies these patients into 5 groups based on the code combination in each discharge record, and the footnote lists all specific procedure codes. If any uncertainty existed, a patient was placed into the “Other” group. The validity of these codes or this grouping has not been examined, but, given the clinical value of these procedures, it is unlikely that the procedure would not be coded in the discharge summary if it were performed, or, conversely, that the procedure would be coded if it were not performed. However, errors in choosing specific codes might occur, therefore some misclassification of patients was expected.
Patient Outcome Measures
Three groups of outcome measures were constructed. The first group included length of stay, hospital charges, and in-hospital deaths, which were available from the source data. The second group was measures of complications or adverse events based on the AHRQ Patient Safety Indicators (PSIs).35 The AHRQ PSIs include 20 indicators with reasonable validity, specificity, and potential for fostering quality improvement. Details on the development and validation of these indicators, the variables and ICD-9-CM codes used to define these PSIs, and the computer programs applying the PSIs to hospital discharge data were downloaded from the AHRQ website.35 Our analysis included the following 6 PSIs of primary concern to patients who undergo cardiac device implantation: iatrogenic pneumothorax (PSI 6), postoperative hemorrhage or hematoma (PSI 9), postoperative pulmonary embolism or deep vein thrombosis (PSI 12), infection caused by medical care (PSI 7), postoperative sepsis (PSI 13), and accidental puncture/laceration (PSI 15). The third group of outcome measures was based on ICD-9-CM codes for mechanical complications caused by PM (99601) or by AICD (99604), recorded in the current hospitalization as a secondary diagnosis. Finally, a composite outcome measure was created to indicate whether a patient had any of the 7 types of complications identified through the PSIs and the ICD-9-CM codes for mechanical complications.
Statistical Method
National estimates on the numbers of cardiac device implantations by patient and hospital characteristics were estimated and tabulated. The diagnoses codes were examined and tabulated. Weighted estimates and standard errors were calculated for patient outcome measures. Student’s t tests were used to determine statistically significant difference between 2 estimates when needed.
We conducted a series of multivariable regressions to explore the relationship between patient outcomes and patient and hospital characteristics such as patient comorbid conditions and hospital volume. General linear regressions were used to estimate the effects of patient and hospital characteristics on continuous outcomes variables (i.e., LOS and costs), and logistic regressions were used to estimate the effects of the characteristics on dichotomous outcomes variables (i.e., mortality and complication measures). P < 0.05 and p < 0.01 were considered statistically significant and highly significant, respectively.
RESULTS
National Estimates of Cardiac Device Implantation and Patient Characteristics
Table 1 shows the national estimates of primary PM, AICD, and CRT systems implanted in 1997 to 2004 in the United States. The last column presents the number of patients who had 1 or more cardiac device procedures but could not be placed with certainty in the first 4 groups. From 1997 through 2004 there was a 145% increase in the yearly number of new AICD implantations, but an increase of only 24% in pacemaker implantations. PM implantations leveled off after 2001 and demonstrated a small decline in 2004. New AICD implants also leveled off a year later, after 2002. After approval by the FDA in 2001, CRT-D and CRT-P implantations increased quickly.
Table 2 displays the associated patient and hospital characteristics for cardiac device implants performed in 2004. Patients aged 65 or over accounted for 70% of CRT patients, 60% of AICD patients, and over 85% of PM patients. Three-quarters of CRT and AICD patients were male, whereas about half of the PM patients were male. Whites accounted for more than half of the patients. At least 75% of the patients had 1 or more chronic conditions. Approximately half of CRT implants were planned admissions, whereas most AICD and PM implants were during emergent admissions. Medicare was billed for three-quarters of all cardiac device implants. Most CRT and AICD implants were performed in large teaching hospitals and hospitals that implanted more than 300 primary PM, AICD, or CRT systems a year. PM implants were most often done in urban nonteaching hospitals, and equally distributed among low, medium, and high-volume hospitals.
More than 60% of patients with a new CRT had congestive heart failure as the principal diagnosis (table available upon request). The proportion of patients who had congestive heart failure as either the principal or a secondary diagnosis was 93%, 88%, 51%, 28%, and 41% in the 5 groups, respectively. Cardiac dysrhythmias were the most frequent primary diagnosis for new AICD and PM implants.
Short-term Patient Outcomes following Cardiac Device Implantations
Table 3 presents the national estimates for short-term patient outcomes for 2004. The length of stay was about 6 days for implanting primary PM, AICD, or CRT systems, but the charges and costs for CRT and AICD implantation were double that for PMs. In-hospital mortality risks were about 1% for CRTs and AICDs and slightly higher for PMs, but the difference was not statistically significant (p > 0.05). The 7 measures of complications each occurred in 1% or fewer of admissions. One or more complications occurred in 2–4% of new implantations. Mechanical complications were substantially more frequently reported in hospitalizations with cardiac device procedures that could not be determined to represent new implantations.
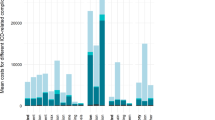
Table 4 highlights selected outcome estimates for AICD patients for the years 1997 to 2003 (tables for other comes and other patient groups available upon request). Mean LOS decreased continuously, whereas charges nearly doubled. In-hospital mortality rates decreased and complication rates fluctuated slightly during the period.
Relationship between Patient Outcomes and Patient and Hospital Characteristics
Table 5 presents the effects of patient and hospital characteristics on in-hospital mortality for the 5 patient groups. Across the 5 patient groups, in-hospital mortality was higher among patients who were older, under Medicare coverage, with more comorbid diseases, or admitted through the emergency department. Smaller hospitals appeared to have lower in-hospital mortality rates, whereas urban teaching hospitals had higher in-hospital mortality rates. The data did not show a consistent volume–mortality relationship across the 5 patient groups.
Table 6 presents the effects of patient and hospital characteristics on occurrence of complications. Again, patient frailty indicated by advanced age and comorbidity was significant. The relationships between other outcome measures and patient and hospital characteristics are not presented, but are available from the authors upon request. Overall, the estimates were similar to that for in-hospital mortality with some notable differences; for example, patients with more comorbid conditions were less likely to suffer from iatrogenic pneumothorax.
DISCUSSION
This study showed steady increases in the number of AICDs and PMs implanted between 1997 and 2001. After the FDA approval of CRT in 2001, the growth in AICDs and PMs leveled off, and CRT implantations rapidly increased. In 2004, about 33,000 new CRT-D, 7,000 CRT-P, 67,000 new AICD, and 179,000 new PM systems were implanted the United States.
A survey of physicians and device companies estimated that 153,000 PMs and 29,000 AICDs were implanted in 1997.5 Our administrative data-based estimates for the same year were 145,000 PMs and 27,000 AICDs, suggesting that administrative data are an alternative to assessment of cardiac device utilization in the United States.
Most patients who underwent cardiac device implantations were elderly whites with multiple chronic conditions. Most patients had principal diagnoses of congestive heart failure, cardiac dysrhythmia, or conduction disorder, and almost 100% of CRT-D patients had a primary or secondary diagnosis of congestive heart failure. These data suggest that administrative data could be used, to some extent, to assess whether cardiac devices are implanted in patients with proper indications. Further studies could be conducted in narrowly defined patient groups to examine patient indications.
Whereas most CRT and AICD implantations were done in large teaching hospitals that implanted 300 or more primary systems a year, PM implants were done more among nonteaching and low-volume hospitals. More research could be conducted to examine how patient characteristics and outcomes differ by hospital type, for example, whether patient outcomes are better in high-volume hospitals than in low-volume hospitals.
Patients stayed in hospitals for about 5 days for AICD implantation in 2004, a substantial decrease from 9.19 days in 1997. In the meantime, the charges and costs increased steadily, from an average charge of $66,530 for an AICD in 1997 to $114,782 in 2004. CRT-D and AICD implantations were substantially more costly than CRT-P and PM. These cardiac device procedures had a substantially lower than average cost-to-charge ratio of 0.50, suggesting that patient admissions for cardiac device procedures might be more profitable than other hospital admissions. The rapid diffusion, especially the increase in CRT implantations, coupled with the profit potential, raises a question about the proper use of these devices.
Fewer than 2% of the patients died, and fewer than 4% of the patients had complications during hospitalization. As expected, iatrogenic pneumothorax was substantially more frequent in cardiac device implantations compared with that in surgical patients, which was reported at 0.09% in 2003,36 whereas the rates of other complications in cardiac device patients were comparable to those in general surgical patients as documented by the 2006 National Healthcare Quality Report, where postoperative hemorrhage or hematoma, DVT/PE, and accidental puncture were reported at 0.2%, 0.9%, and 0.4%, respectively.36 Our analysis further showed that adverse outcomes were mostly associated with patient frailty indicated by advanced age, comorbidities, and emergency admission, and associated with the complexity of device implantations (i.e., AICDs and CRTs compared to pacemaker implantations). Given that the patients were mostly elderly with multiple chronic conditions, these low risks of death and complications suggest that the implantation procedures were fairly safe.
Administrative data have many limitations when used to study a clinical intervention. Previous studies identified many cardiac device-related complications, such as pocket hematoma,15,37,38 pocket infections,7,38–43 iatrogenic pneumothorax,40,41 arterial puncture,40 venous thrombosis and stenosis,41 electrode displacement,40 lead dislodgements, undersensing,40,42 cardiac device endocarditis,44,45 interference by an electronic antitheft-surveillance device46 or a Personal Digital Assistant,17 and twiddle-induced torsion of leads.41 Administrative data may not able to identify many of these specific types of complications. The data do not capture deaths or complications that are detected after discharge. The data do not capture the risk associated with the experience of the surgeon, type of device used (such as dual-chamber pacemaker or biventricular pacemaker, both of which have different risks of complications),47 the experience of operating room staff, type of anesthesia used, and other clinical variables. Nevertheless, our study demonstrates that administrative data provide an efficient and reliable source to track utilization of cardiac devices, to evaluate associated patient and hospital characteristics, and to offer valuable insights into patient risks and outcomes after implantations.
References
Maisel WH. Cardiovascular device development: lessons learned from pacemaker and implantable cardioverter-defibrillator therapy. Am J Ther. 2005;12(2):183–5.
Pavia S, Wilkoff B. The management of surgical complications of pacemaker and implantable cardioverter-defibrillators. Curr Opin Cardiol. 2001;16(1):66–71.
Goldberger Z, Lampert R. Implantable cardioverter-defibrillators: expanding indications and technologies. JAMA. 2006;295(7):809–18.
Bernstein AD, Parsonnet V. Survey of cardiac pacing and defibrillation in the United States in 1993. Am J Cardiol. 1996;78(2):187–96.
Bernstein AD, Parsonnet V. Survey of cardiac pacing and implanted defibrillator practice patterns in the United States in 1997. Pacing Clin Electrophysiol. 2001;24(5):842–55.
Daley WR, Kaczmarek RG. The epidemiology of cardiac pacemakers in the older US population. J Am Geriatr Soc. 1998;46(8):1016–9.
Cabell CH, Heidenreich PA, Chu VH, et al. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J. 2004;147(4):582–6.
Maisel WH, American Cardiology C, American Heart A, North American Society of Pacing and Electrophysiology. Impact of expanding indications on the safety of pacemakers and defibrillators. Cardiac Electrophysiology Review. 2003;7(1):30–2.
Bradley DJ, Bradley EA, Baughman KL, et al. Cardiac resynchronization and death from progressive heart failure: a meta-analysis of randomized controlled trials. JAMA. 2003;289(6):730–40.
Bax JJ, Abraham T, Barold SS, et al. Cardiac resynchronization therapy. Part 2: Issues during and after device implantation and unresolved questions. J Am Coll Cardiol. 2005;46(12):2168–82.
Leon AR, Abraham WT, Curtis AB, et al. Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: combined results of over 2,000 patients from a multicenter study program. J Am Coll Cardiol. 2005;46(12):2348–56.
Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352(15):1539–49.
Young JB, Abraham WT, Smith AL, et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA. 2003;289(20):2685–94.
Wiegand UK, Bode F, Bonnemeier H, Eberhard F, Schlei M, Peters W. Long-term complication rates in ventricular, single lead VDD, and dual chamber pacing. Pacing Clin Electrophysiol. 2003;26(10):1961–9.
Wiegand UK, LeJeune D, Boguschewski F, et al. Pocket hematoma after pacemaker or implantable cardioverter defibrillator surgery: influence of patient morbidity, operation strategy, and perioperative antiplatelet/anticoagulation therapy. Chest. 2004;126(4):1177–86.
Rozmus G, Daubert JP, Huang DT, Rosero S, Hall B, Francis C. Venous thrombosis and stenosis after implantation of pacemakers and defibrillators. Journal Interventional Cardiac Electrophysiology. 2005;13(1):9–19.
Tri JL, Trusty JM, Hayes DL. Potential for Personal Digital Assistant interference with implantable cardiac devices. Mayo Clin Proc. 2004;79(12):1527–30.
Sweeney MO, Shea JB, Ellison KE. Upgrade of permanent pacemakers and single chamber implantable cardioverter defibrillators to pectoral dual chamber implantable cardioverter defibrillators: indications, surgical approach, and long-term clinical results. Pacing Clin Electrophysiol. 2002;25(12):1715–23.
Maisel WH. Pacemaker and ICD generator reliability: meta-analysis of device registries. JAMA. 2006;295(16):1929–34.
Hammill S, Phurrough S, Brindis R. The national ICD registry: now and into the future. Heart Rhythm. 2006;3(4):470–3.
NCC-NCDR National Cardivascular Data Registry, ICD Registry. Available at http://www.accncdr.com/webncdr/ICD/Default.aspx; Accessed Nov. 1, 2006.
Maisel WH, Moynahan M, Zuckerman BD, et al. Pacemaker and ICD generator malfunctions: analysis of Food and Drug Administration annual reports. JAMA. 2006;295(16):1901–6.
Wilkoff BL. Pacemaker and ICD malfunction—an incomplete picture. JAMA. 2006;295(16):1944–6.
Gould PA, Krahn AD. Complications associated with implantable cardioverter-defibrillator replacement in response to device advisories. JAMA. 2006;295(16):1907–11.
Maisel WH, Stevenson WG, Epstein LM. Changing trends in pacemaker and implantable cardioverter defibrillator generator advisories. Pacing Clin Electrophysiol. 2002;25(12):1670–8.
Maisel WH, Sweeney MO, Stevenson WG, Ellison KE, Epstein LM. Recalls and safety alerts involving pacemakers and implantable cardioverter-defibrillator generators. [See comment]. JAMA. 2001;286(7):793–99.
Bernstein AD, Parsonnet V. Survey of cardiac pacing in the United States in 1989. Am J Cardiol. 1992;69(4):331–8.
Mond HG, Irwin M, Morillo C, Ector H. The world survey of cardiac pacing and cardioverter defibrillators: calendar year 2001. Pacing Clin Electrophysiol. 2004;27(7):955–64.
Zhan C, Miller M. Administrative data-based patient safety research: a critical review. Quality and Safety of Health Care. 2003;12(Suppl II):II58–II63.
Agency for Healthcare Research and Quality. Healthcare Cost & Utilization Project. Available at http://www.ahrq.gov/data/hcup/ Accessed July 20, 2006.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Curtis AB, Ellenbogen KA, Hammill SC, et al. Clinical competency statement: training pathways for implantation of cardioverter defibrillators and cardiac resynchronization devices. [See comment]. Heart Rhythm. 2004;1(3):371–5.
Tobin K, Stewart J, Westveer D, Frumin H. Acute complications of permanent pacemaker implantation: their financial implication and relation to volume and operator experience. Am J Cardiol. 2000;85(6):774–6.
Parsonnet V, Bernstein AD, Lindsay B. Pacemaker-implantation complication rates: an analysis of some contributing factors. J Am Coll Cardiol. 1989;13(4):917–21.
Agency for Healthcare Research and Quality. Guide to Patient Safety Indicators. Available at: http://www.qualityindicators.ahrq.gov/psi_download.htm. Accessed July 20, 2006. Rockville, MD: Agency for Healthcare Research and Quality; 2006.
Agency for Healthcare Research and Quality. National Healthcare Quality Report, 2006. Available at: http://www.ahrq.gov/qual/nhqr06/index.html#Safety. Accessed April 17, 2007. Rockville, MD: Agency for Healthcare Research and Quality, 2006.
Gupta A, Zegel HG, Dravid VS, Nierenberg SJ, Freiman DB. Value of radiography in diagnosing complications of cardioverter defibrillators implanted without thoracotomy in 437 patients. AJR Am J Roentgenol. 1997;168(1):105–8.
Pfeiffer D, Jung W, Fehske W, et al. Complications of pacemaker-defibrillator devices: diagnosis and management. Am Heart J. 1994;127(4 Pt 2):1073–80.
Harcombe AA, Newell SA, Ludman PF, et al. Late complications following permanent pacemaker implantation or elective unit replacement. Heart. 1998;80(3):240–4.
Aggarwal RK, Connelly DT, Ray SG, Ball J, Charles RG. Early complications of permanent pacemaker implantation: no difference between dual and single chamber systems. Br Heart J. 1995;73(6):571–5.
Jones GK, Bardy GH, Kudenchuk PJ, et al. Mechanical complications after implantation of multiple-lead nonthoracotomy defibrillator systems: implications for management and future system design. Am Heart J. 1995;130(2):327–33.
Kiviniemi MS, Pirnes MA, Eranen HJ, Kettunen RV, Hartikainen JE. Complications related to permanent pacemaker therapy. Pacing Clin Electrophysiol. 1999;22(5):711–20.
Da Costa A, Kirkorian G, Cucherat M, et al. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation. 1998;97(18):1796–801.
del Rio A, Anguera I, Miro JM, et al. Surgical treatment of pacemaker and defibrillator lead endocarditis: the impact of electrode lead extraction on outcome. Chest. 2003;124(4):1451–9.
Klug D, Lacroix D, Savoye C, et al. Systemic infection related to endocarditis on pacemaker leads: clinical presentation and management. Circulation. 1997;95(8):2098–107.
Santucci PA, Haw J, Trohman RG, Pinski SL. Interference with an implantable defibrillator by an electronic antitheft-surveillance device. N Engl J Med. 1998;339(19):1371–4.
Link MS, Estes NA 3rd, Griffin JJ, et al. Complications of dual chamber pacemaker implantation in the elderly. Pacemaker Selection in the Elderly (PASE) Investigators. Journal of Interventional Cardiac Electrophysiology. 1998;2(2):175–9.
Acknowledgments
The authors thank Zhengyi Fang, Social and Scientific Systems, Inc., for excellent computing support. We thank Parivash Nourjah, PhD, and Joyce Basu, PhD, the Agency for Healthcare Research and Quality, for useful comments. The authors would also like to acknowledge the statewide data organizations that participate in the HCUP Nationwide Inpatient Sample: California Office of Statewide Health Planning & Development; Colorado Health & Hospital Association; Connecticut - Chime, Inc.; Florida Agency for Health Care Administration; Georgia—GHA: An Association of Hospitals & Health Systems; Hawaii Health Information Corporation; Illinois Department of Public Health; Iowa Hospital Association; Kansas Hospital Association; Kentucky Department for Public Health; Maine Health Data Organization; Maryland Health Services Cost Review Commission; Massachusetts Division of Health Care Finance and Policy; Michigan Health and Hospital Association; Minnesota Hospital Association; Missouri Hospital Industry Data Institute; Nebraska Hospital Association; Nevada Department of Human Resources; New Jersey Department of Health & Senior Services; New York State Department of Health; North Carolina Department of Health and Human Services; Ohio Hospital Association; Oregon Association of Hospitals & Health Systems; Pennsylvania Health Care Cost Containment Council; Rhode Island Department of Health; South Carolina State Budget & Control Board; South Dakota Association of Healthcare Organizations; Tennessee Hospital Association; Texas Health Care Information Council; Utah Department of Health; Vermont Association of Hospitals and Health Systems; Virginia Health Information; Washington State Department of Health; West Virginia Health Care Authority; Wisconsin Department of Health & Family Services.
Disclaimer
The authors of this article are responsible for its contents. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality, the U.S. Department of Health and Human Services.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
APPENDIX
APPENDIX
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Zhan, C., Baine, W.B., Sedrakyan, A. et al. Cardiac Device Implantation in the United States from 1997 through 2004: A Population-based Analysis. J GEN INTERN MED 23 (Suppl 1), 13–19 (2008). https://doi.org/10.1007/s11606-007-0392-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0392-0